Transplantation Genomics: The Bridesmaid Behind the Scenes of Human “Organ Matching”
In our bodies, each organ has its identity card. When an organ goes on strike and needs to be replaced, it is not just a matter of finding a spare tyre. In organ transplantation, like a high-profile blind date, the key is the new “members” must be recognised by the body's immune system. Otherwise, it will be treated as a foreign enemy, and the immune cells will be attacked, making a sensational “rejection reaction”. This “ultimate blind date” for transplantation matching is as difficult as finding the perfect soul mate. Transplantation genomics is the “super bride” that controls everything behind the scenes, using genetic data to accurately predict who will be a “match made in heaven”.

The immune system is the most critical “mother-in-law” in this matchmaking event, responsible for vetting all the “new members” entering the body. One of its criteria is the HLA gene system, a set of genes that determines an individual's “identity card”. It is important to realise that the degree of HLA match directly affects the success of the transplant. The better the match, the easier it is for the immune system to nod its head in agreement, and the two sides can coexist peacefully; if the match fails, the rejection reaction can be staged at any time “palace drama”, just like you can't just put a cat in a kennel and expect them to be at peace with each other.
The role of genomics here is like a bride with a powerful database. It will come up with a “genetic resume” of the donor and the recipient, and through whole genome sequencing technology, it will compare the HLA typing and genetic differences of both parties one by one, and it can even predict the possible problems in the future. It's like investigating a person's circle of friends, ex-history and credit report before falling in love. This kind of precise analysis makes the match more scientific, avoiding the tragedy of “falling in love and killing each other” after hitting it off.
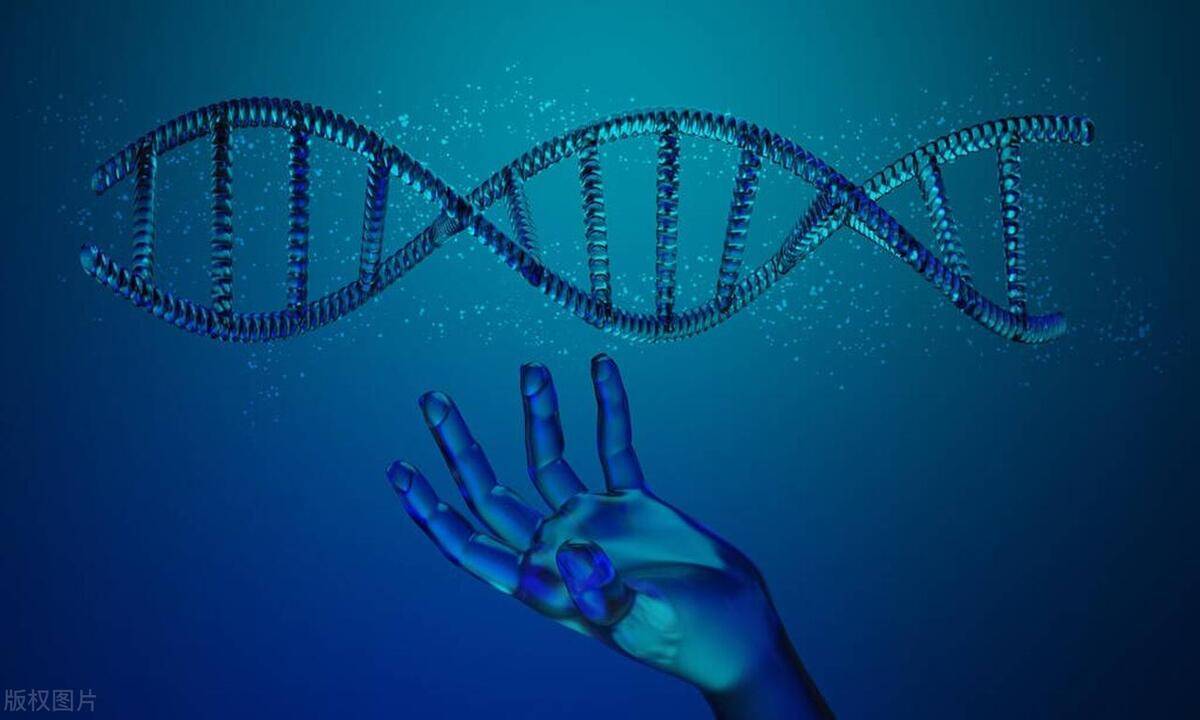
Future transplantation technology may even skip the step of “matchmaking” and directly realise “customised partners”. Gene editing technology is like an all-purpose bartender, adjusting the genes of the donor organ in advance, eliminating those “risk factors” that may trigger rejection. Scientists get a “wild” organ and transform it into a “perfect match” for the recipient's body through gene editing. This is not only precision medicine but also a highly customised version of “private ordering”.

In the wide world of medical progress, transplantation genomics is opening the way to a new level of personalised medicine. It is as if you were an architect designing your dream home, from the foundation to every tile on the roof, all crafted to your exact specifications. Now, apply this concept to the field of organ transplantation. The combination of stem cell technology and the genome is like having a top-notch team of “architects of life” who can grow an organ in a lab that is a perfect match for you based on your DNA blueprint. It's like having the perfect customised “spare parts for life” that harmonise with your body inside and out. In the future, as the technology matures and becomes more widespread, everyone can expect to have a replacement organ that is genetically identical to their own.
Of course, the road to transplantation is not a straight one. Privacy of genetic data is a major challenge, as is the cost of the technology. In addition, the high cost of the technology is like a boulder on the road to recovery, deterring many eager souls from seeking a new life. What is more complicated is that the ethical issues touched by gene editing, especially the boundary of “modifying life”, have triggered extensive controversy and deep thinking in all walks of life. We are standing at the crossroads of morality and science, and we need to be cautious at every step so as not to step into an unknown ethical minefield. But in any case, genomics is leading us to an era of higher transplantation success and lower rejection. It is like an insightful bride, ensuring that transplantation is a safer and more efficient “organ match” so that more patients can have the hope of a second life.
(Writer:Weink)