CRISPR Therapy Global Rollout: Casgevy's Impact on Sickle Cell Anemia Treatment
In January 2025, England’s National Health Service (NHS) made history by approving Casgevy—the world’s first CRISPR-based gene therapy for severe sickle cell anemia (SCA)—marking a turning point for a disease that afflicts 100,000 people in the U.S., 25,000 in Europe, and 30 million globally, per World Health Organization (WHO) data. This milestone followed its 2023 approvals by the U.S. FDA and European Medicines Agency (EMA), shifting CRISPR from experimental science to life-saving clinical practice. As Vertex Pharmaceuticals (co-developer with CRISPR Therapeutics) expands its network of authorized treatment centers—now 12 in the U.S., three in Western Europe, one in Saudi Arabia, and a newly announced site in Canada (March 2025)—the therapy’s global rollout reveals both the transformative power of gene editing and the stubborn barriers to equitable access.
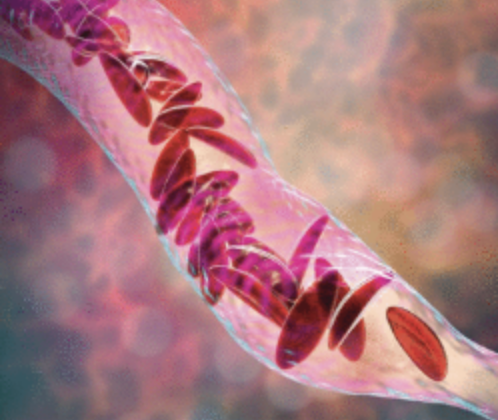
Casgevy’s mechanism targets the genetic root of SCA: it edits the BCL11A gene in a patient’s own blood stem cells (collected via apheresis), reactivating production of fetal hemoglobin—a protein that bypasses the defective adult hemoglobin causing red blood cells to “sickle” and block blood vessels. Clinical data presented at the 2024 European Hematology Association Congress underscores its game-changing efficacy: 92.3% of 132 treated patients remained free from painful vaso-occlusive crises (the most debilitating SCA symptom) for at least 12 consecutive months, compared to a pre-treatment average of 3.5 crises yearly. For 27-year-old U.S. patient Maya Carter, who endured 10 hospitalizations annually before treatment in 2022, the difference is stark: “I haven’t missed a day of work in two years. This isn’t just a therapy—it’s a second life.” Long-term follow-up, published in The Lancet Haematology in early 2025, shows 89% of patients retained these benefits at five years, with no evidence of CRISPR-related off-target effects.
The global expansion, however, proceeds along starkly unequal lines. In the U.S., Casgevy carries a wholesale price of two million two hundred thousand United States dollars—offset partially by Vertex’s patient support programs, which cover out-of-pocket costs for 78% of insured patients. By contrast, the UK’s NHS secured access after negotiating a confidential discounted rate, with treatment now available at three specialist hubs (London, Manchester, Birmingham) for eligible adults and adolescents. Europe’s rollout is fragmented: Germany approved Casgevy in February 2025 but limits access to university hospitals, while France is still finalizing reimbursement terms. Saudi Arabia, which approved the therapy in late 2024, has emerged as a regional leader, treating 15 patients in Riyadh’s King Faisal Specialist Hospital—reflecting growing demand beyond Western markets. Vertex aims to scale to 50 U.S. centers and 25 European sites by 2026, but this lags behind competitor Bluebird Bio’s Lyfgenia, which already has 40 U.S. locations.
Accessibility remains the most pressing challenge. While high-income countries navigate cost debates (lifetime SCA treatment—including hospitalizations, transfusions, and pain meds—averages four million to six million United States dollars, justifying the one-time therapy expense), low-income nations face infrastructure collapse. Nigeria, which accounts for 40% of global SCA births (200,000 yearly), has only one pilot program (at Lagos University Teaching Hospital) funded by the Bill & Melinda Gates Foundation. The therapy’s logistical hurdles—patient-specific stem cell editing requires 2–3 weeks of lab work, plus cryogenic transport—further limit scalability. To address this, WHO launched the “CRISPR for SCD” alliance in March 2025, partnering with Vertex and local African labs to train 100 researchers in stem cell processing by 2027.
Recent safety data continues to reassure: Vertex’s Q1 2025 report on 200 patients showed no long-term complications beyond typical transplant risks (like infection). As Dr. Jane Nkala, a Zambian hematologist and WHO advisor, notes: “Casgevy proves we can cure SCA—but cure means nothing if only 1% of patients can access it.” The therapy’s global journey is thus a dual story: a triumph of precision medicine, and a test of whether the world can deliver innovation equitably. For millions living with SCA, Casgevy is more than a breakthrough—it’s a promise that the future of medicine must leave no one behind.
(Writer:Galli)

